Member Resources The Value of TrueCost. Prior Authorization Form for Medical Procedures Courses of Treatment or Prescription Drug Benefits 69O-161011 OIR-B2-2180 New 1216 Capital Health Plan PO.

43 Credit Card Authorization Forms Templates Ready To Use
If so your EOC will be included on the letter.

. Claims Processing Adjudication Giving You Freedom to Focus. 1 PDF editor e-sign platform data collection form builder solution in a single app. Custom design benefits prior authorization form.
Digitize the current prior authorization process For those health systems and practices looking to at least free themselves from faxes phone calls and endless email loops digitizing claims management can be a small step forward in automating prior auth and reducing denied claimsThis might involve something as simple as a web portal that allows providers to create. Call our Provider Unit today at 877-625-0205. Here you will be able to check eligibility benefits and preauthorization requirements.
For questions on eligibility and benefits call. On the prior authorization form the person making the request must provide. This tool does not apply for members of the Federal Employee Program or PAI plans Fax.
Follow the step-by-step instructions below to design your group benefits drug prior authorization dynamic lifecycle form that can flip languages wig. Standard Commercial Prior Authorization Request Form - West Virginia Created Date. 3 This form does not replace payer specific prior authorization requirements.
You can access your portal 247 or contact us. TrueCost by CDB is designed to deliver the highest quality benefits at an affordable cost to you. ESI is the pharmacy benefits manager for Maryland Physicians Care.
A typed drawn or uploaded signature. Prior Authorizations EOC ID. Box 15349 Tallahassee FL 32317 Medication Management Medications.
We lead clients to substantial savings through TrueCost Rx and our specialty drug prior authorization services. Create a custom prestige prior authorization form 0 that meets your industrys specifications. A non-preferred drug is a drug that is not listed on the Preferred Drug List PDL of a given insurance provider or State.
Prior Authorization Form Supporting clinical documentation may be requested to ascertain benefit coverage determination. To request preauthorization by fax please complete the appropriate preauthorization request form. First name last name and date of birth of the member.
We keep our process simple with TrueCosts unique copay-only plan design that removes the complexity from the payment process and eliminates coinsurance and deductibles. The prescription benefit is one of the most important and controllable elements of an employers benefit plan. Providers can access the Formulary Search Tool to find additional information about medications or call ESI directly at 1-800-753-2851.
Create Legally Binding Electronic Signatures on Any Device. If you have any questions contact EHIMs Department of Clinical Services at 248 948-9900 or fax us at 248 948-9904. Summaries or CPT and ICD-9 codes.
Eligibility Must Be Verified At Time Services Are Rendered. If you fax your request to CBA keep a copy of the faxed. Select the document you want to sign and click Upload.
Plan benefits are based on the patients eligibility at the time of service. We custom design pharmacy benefit plans that ensure your Members receive the best prescription benefits at the lowest. Submit an extension request prior to the end of the authorization period.
Our approach is personalized and. A unique number assigned to the PA request. 2019 festival hong program.
URGENT Three business days Routine RETRO. 2 Not all services listed will be covered by the benefits in a members health plan product. H4140_MMOD_C Submit all requests via fax.
Authorization Does Not Guarantee Payment. Its available to you 24 hours a day. Payment is subject to benefit coverage rules including member eligibility and any contractual limitations in effect at the time of service.
Our hours of operation are 800 am to 500 pm EST. We also work with our clients to develop direct contracting specialty networks and cost plus models. We know you need to focus on the important work of caring for your clients.
26711 Northwestern Highway Suite 400 Southfield MI 48033. Decide on what kind of signature to create. You can find this by calling the Prior Authorization line at 8886088851 or.
Prescription prior authorization forms are used by physicians who wish to request insurance coverage for non-preferred prescriptions. The standardized prior authorization form is intended to be used to submit prior authorizations requests by fax or mail. Partnering with Elixir you get 15 years of proven experience and you dont have to sacrifice quality for cost.
Ad pdfFiller allows users to edit sign fill and share all type of documents online. Hong kong arts festival 2019 program. Prescription prior authorization forms are used by physicians who wish to reque Written By lion Saturday April 23 2022 Add Comment Edit.
Custom Design Benefits Providers may use the Provider Portal to. Prior Rx Authorization Forms. Employee Health Insurance Management Inc.
As a reminder authorization is not a guarantee of payment. Prior authorization requests for covered outpatient medications are processed through Express Scripts Inc. Provider Resources Download Forms.
They need prescriptions filled quickly and accurately and were here to helpLet us worry about managing the claims adjudications and processing prescription benefits call center troubleshooting and other administrative tasks that can. Standard Prior Authorization Request Form - West Virginia Author. To meet the needs of our clients BAS has access to over 50 local regional and national provider networks allowing us to provide deeper discounts and better access.
Prior authorization is not a guarantee of payment. Ad signNow allows users to edit sign fill and share all type of documents online. There are three variants.
Custom Design Benefits CDB has been pioneering a new direction through self-funding strategic cost containment and benefit plans designed to work for your workforce. You may have received a letter regarding this particular prior authorization. MMFAXCUSTOMDESIGNBENEFITSCOM OR FAX TO 513-389-2997 This authorization is not a guarantee of payment.

Credit Card Authorization Form Template Jotform

Release Of Information Template Pdf Templates Jotform
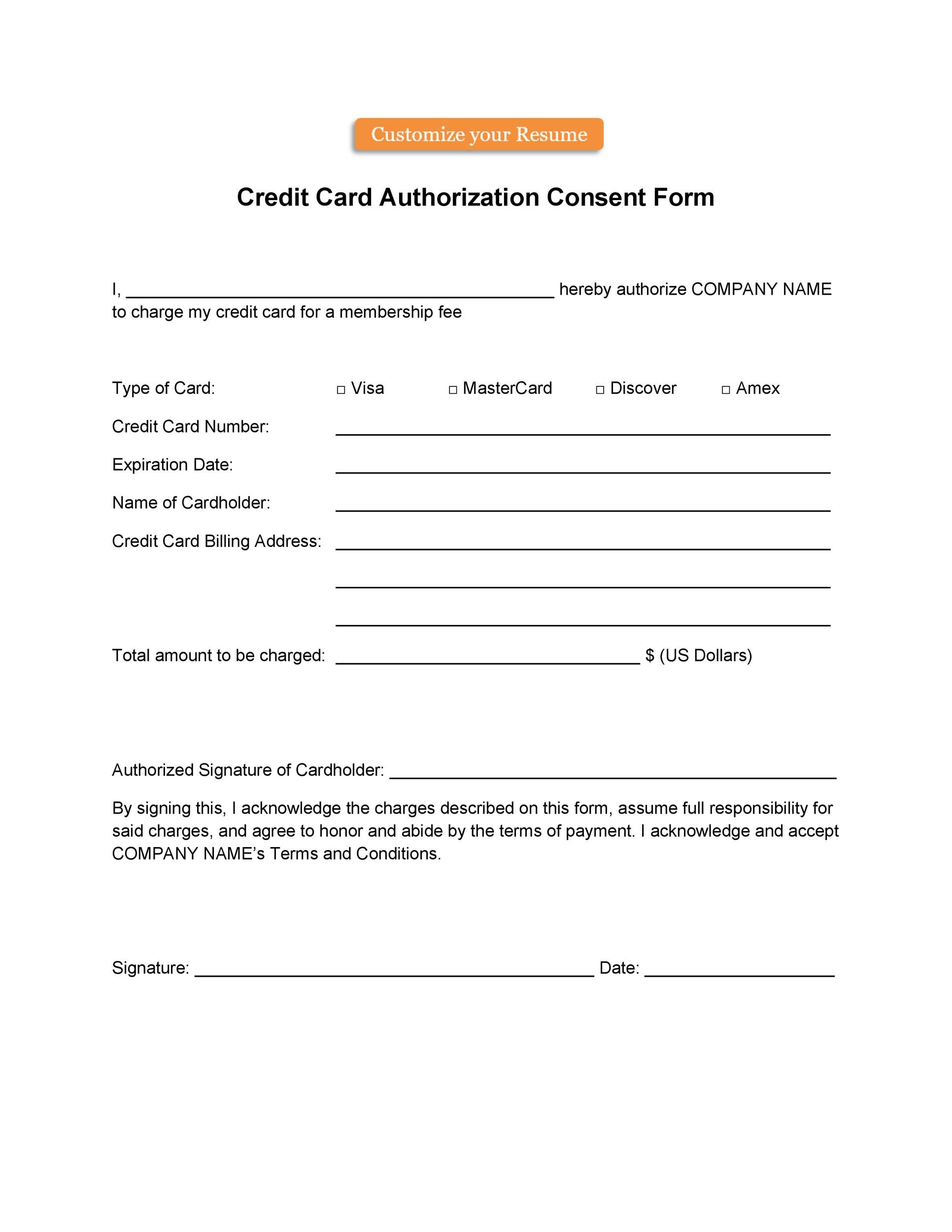
43 Credit Card Authorization Forms Templates Ready To Use

Consent Forms Form Templates 123formbuilder

Direct Deposit Authorization Pdf Templates Jotform

Free 23 Insurance Verification Forms In Pdf Dental Insurance Dental Insurance Plans Dental

0 comments
Post a Comment